Moscow Center of Advanced Sports Technologies (Sports Psychology Department, physiologist)
Moscow, Russian Federation
Moscow, Russian Federation
VAK Russia 5.3.2
VAK Russia 1.1.10
VAK Russia 1.2.1
VAK Russia 1.2.2
VAK Russia 1.2.3
VAK Russia 1.5.2
VAK Russia 1.5.8
VAK Russia 3.3.9
VAK Russia 3.1.33
VAK Russia 5.2.3
VAK Russia 5.2.6
VAK Russia 5.3.4
VAK Russia 5.8.4
VAK Russia 5.8.5
VAK Russia 5.8.6
VAK Russia 5.8.7
VAK Russia 5.6.6
VAK Russia 5.12.1
VAK Russia 5.12.4
UDC 57.089
UDC 612
UDC 159.91
UDC 52-17
UDC 347.514.3
UDC 00
UDC 31
CSCSTI 00.77
CSCSTI 77.00
CSCSTI 14.00
CSCSTI 20.00
CSCSTI 83.00
Russian Classification of Professions by Education 02.00.00
Russian Classification of Professions by Education 06.00.00
Russian Classification of Professions by Education 09.00.00
Russian Classification of Professions by Education 32.00.00
Russian Classification of Professions by Education 39.00.00
Russian Classification of Professions by Education 44.00.00
Russian Library and Bibliographic Classification 1
Russian Library and Bibliographic Classification 22
Russian Library and Bibliographic Classification 28
Russian Library and Bibliographic Classification 3
Russian Library and Bibliographic Classification 58
Russian Library and Bibliographic Classification 73
Russian Library and Bibliographic Classification 74
Russian Library and Bibliographic Classification 75
Russian Trade and Bibliographic Classification 5
Russian Trade and Bibliographic Classification 7
BISAC SEL SELF-HELP
BISAC COM014000 Computer Science
BISAC COM072000 Computer Simulation
BISAC COM017000 Cybernetics
BISAC COM018000 Data Processing
BISAC COM062000 Data Modeling & Design
BISAC COM089000 Data Visualization
BISAC COM021000 Databases / General
BISAC COM021030 Databases / Data Mining
BISAC COM023000 Educational Software
BISAC COM025000 Expert Systems
BISAC COM074000 Hardware / Mobile Devices
BISAC COM080000 History
BISAC COM079010 Human-Computer Interaction (HCI)
BISAC COM032000 Information Technology
BISAC COM031000 Information Theory
BISAC COM004000 Intelligence (AI) & Semantics
BISAC COM060000 Internet / General
BISAC COM039000 Management Information Systems
BISAC COM077000 Mathematical & Statistical Software
BISAC COM051000 Programming / General
BISAC COM051300 Programming / Algorithms
BISAC COM012040 Programming / Games
BISAC COM060170 Web / Content Management Systems
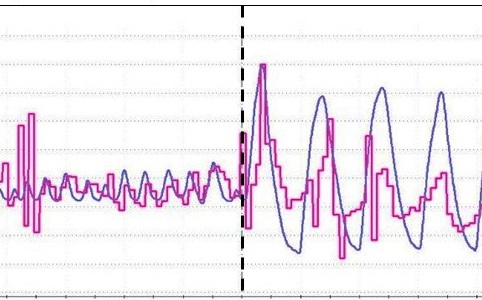
Introduction. The rhythm of the heart (heart rate, HR) is closely related to the rhythm of breathing. The phenomenon of respiratory sinus arrhythmia (an increase in heart rate during inhalation and a decrease during exhalation) is well known. Cardiorespiratory interactions and synchronization of these two signals are evaluated differently in the literature. The purpose of this work was to propose and test an approach to assess cardiorespiratory synchronization – the calculation of the cross-correlation coefficient between heart rate and respiration curve, for a more objective characterization of an athlete’s bodily states. Methods. A photoplethysmogram and respiration were recorded in 45 healthy athletes (18-25 years old) in three situations: rest, paced breathing at 6 times per minute (resonant frequency) and the performance of a sensorimotor task (tapping with the rhythmic metronome sounds and then reproducing a given rhythm from memory). For the HR and respiration curves, filtering and smoothing algorithms using the Savitsky-Goley method were applied sequentially, and then the cross-correlation coefficient between the two curves was calculated. The spectral parameters of heart rate variability (LF and HF) were also obtained, since during spontaneous breathing its contribution to the HR is reflected in HF band, and when breathing at a resonant frequency, a peak occurs at a frequency of 0.1 Hz in the LF band. Results. The cross-correlation coefficient, as well as the peak of HR spectral power at 0.1 Hz, increases significantly when breathing at a resonant frequency. The relationship between these indicators is most accurately described not by a linear, but by a logarithmic dependence. When performing a sensorimotor task, the so-called respiratory waves in the heart rhythm spectrum (HF) do not change from rest to tapping by a metronome and then to holding the rhythm by memory. At the same time, the cross-correlation coefficient demonstrates significant changes between these situations. In addition, a significant correlation was found between the change in the cross-correlation coefficient and the stability of rhythm maintenance (from memory): an increase in the cardiorespiratory synchronization leads to a decrease in motor rhythm stability. Conclusion. Assessment of cardiorespiratory synchronization due to the peculiarities of both signals (changes in heart rate and respiratory phases) requires preliminary preparation of data arrays: filtering and smoothing the stepped curve of heart rate dynamics. The calculation of the cross-correlation coefficient can be used to assess cardiorespiratory synchronization in real time and is likely to be applicable in short time fragments to assess emotional reactions and other short-term fluctuations in psychophysiological conditions, where the classical method of assessing changes in heart rhythm in the frequency or time domains is not applicable.
cardiorespiratory synchronization, heart rate, respiratory sinus arrhythmia, heart rate variability, resonant breathing, spectral analysis, emotional reactions, psychophysiological conditions
1. Dick T.E., Hsieh Y.H., Dhingra R.R., Baekey D.M., Gal´an R.F., Wehrwein E., Morris K.F. Cardiorespiratory coupling: common rhythms in cardiac, sympathetic, and respiratory activities. Progress in brain research, 209, 2014, pp. 191-205. DOI: https://doi.org/10.1016/B978-0-444-63274-6.00010-2
2. Lehrer P.M., Vaschillo E., Vaschillo B. Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Applied psychophysiology and biofeedback, 25(3), 2000, pp. 177-191. DOI: https://doi.org/10.1023/A:1009554825745
3. Gevirtz R. The promise of heart rate variability biofeedback: Evidence-based applications. Biofeedback, 41(3), 2013, pp. 110-120. DOI: https://doi.org/10.5298/1081-5937-41.3.01
4. Shaffer F., McCraty R., Zerr C.L. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Frontiers in psychology, 5, 2014, Article 1040. DOI: https://doi.org/10.3389/fpsyg.2014.01040
5. McCraty R., Shaffer F. Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Global advances in health and medicine, 4(1), 2015, pp. 46-61. DOI: https://doi.org/10.7453/gahmj.2014.073
6. Lehrer P., Vaschillo B., Zucker T., Graves J., Katsamanis M., Aviles M., Wamboldt F. Protocol for heart rate variability biofeedback training. Biofeedback (Online), 41(3), 2013, p. 98-109. DOI: https://doi.org/10.5298/1081-5937-41.3.08
7. McCraty R., Atkinson M., Tomasino D., Bradley R.T. The coherent heart heart-brain interactions, psychophysiological coherence, and the emergence of system-wide order. Integral Review: A Transdisciplinary & Transcultural Journal for New Thought, Research, & Praxis, 5(2), 2009.
8. Camm A.J., Malik M., Bigger J.T., Breithardt G., Cerutti S., Cohen R.J., Singer D. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use, 93(5), 1996, pp. 1043-1065. DOI: https://dx.doi.org/10.1161/01.CIR.93.5.1043
9. Shaffer F., Ginsberg J.P. An overview of heart rate variability metrics and norms. Frontiers in public health, 5, 2017, Article 258. DOI: https://doi.org/10.3389/fpubh.2017.00258
10. Thomas B.L., Claassen N., Becker P., Viljoen M. Validity of commonly used heart rate variability markers of autonomic nervous system function. Neuropsychobiology, 78(1), 2019, pp. 14-26. DOI: https://doi.org/10.1159/000495519
11. Noulhiane M., Mella N., Samson S., Ragot R., Pouthas V. How emotional auditory stimuli modulate time perception. Emotion, 7(4), 2007, pp. 697-704. DOI: https://doi.org/10.1037/1528-3542.7.4.697
12. Mella N., Conty L., Pouthas V. The role of physiological arousal in time perception: psychophysiological evidence from an emotion regulation paradigm. Brain and cognition, 75(2), 2011, pp. 182-187. DOI: https://doi.org/10.1016/j.bandc.2010.11.012
13. Shaffer F., Venner J. Heart Rate Variability Anatomy and Physiology. Biofeedback, 41, 2013, pp. 13-25. DOI: https://doi.org/10.5298/1081-5937-41.1.05
14. Hegarty-Craver M., Gilchrist K.H., Propper C.B., Lewis G.F., DeFilipp S.J., Coffman J.L., Willoughby M.T. Automated respiratory sinus arrhythmia measurement: Demonstration using executive function assessment. Behavior research methods, 50(5), 2018, pp. 1816-1823.
15. Schafer C., Rosenblum M G., Abel H.H., Kurths J. Synchronization in the human cardiorespiratory system. Physical Review E, 60(1), 1999, p. 857-870. DOI: https://doi.org/10.1103/PhysRevE.60.857
16. Zhang J., Yu X., Xie D. Effects of mental tasks on the cardiorespiratory synchronization. Respiratory physiology & neurobiology, 170(1), 2010, pp. 91-95. DOI: https://doi.org/10.1016/j.resp.2009.11.003
17. Schwerdtfeger A.R., Schwarz G., Pfurtscheller K., Thayer J.F., Jarczok M.N., Pfurtscheller G. Heart rate variability (HRV): From brain death to resonance breathing at 6 breaths per minute. Clinical Neurophysiology, 131(3), 2020, pp. 676-693. DOI: https://doi.org/10.1016/j.clinph.2019.11.013